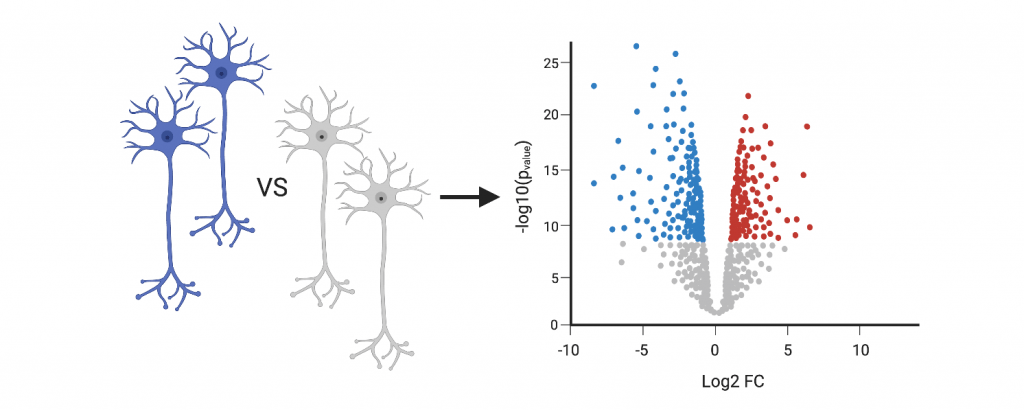
Tauopathies may occur by familial mechanisms in which mutations in the MAPT gene are dominantly inherited causing frontotemporal lobar degeneration (FTLD-tau) or by sporadic mechanisms in which MAPT haplotypes are associated with increased disease risk (e.g. progressive supranuclear palsy and corticobasal degeneration). MAPT mutations and risk haplotypes have been proposed to drive disease pathogenesis through proteoforms that contain 3-microtubue binding domain repeats (3R tau), 4R tau, or both. However, the mechanisms by which tauopathies occur remains poorly understood. We propose that MAPT mutations drive tau aggregation and neuronal dysfunction through altered proteostasis. In preliminary studies, we have shown that induced pluripotent stem cell derived-neurons expressing MAPT mutations exhibit changes in tau turnover compared to isogenic, control neurons, and we observed differences in the turnover of specific tau proteoforms in mutant neurons. Neurons expressing MAPT mutations exhibit enlarged lysosomal structures and secondary elevation of lysosomal enzymes, markers of lysosomes that are unable to properly degrade their contents. Correction of the mutant allele was sufficient to restore these lysosomal defects. This suggests that altered tau kinetics may be due to defects in the endolysosomal pathway. Thus, a unifying feature by which MAPT mutations drive tauopathy is through disrupted proteostasis. The objective of this study is to extend our preliminary findings to manipulate tau proteoforms using genetic or molecular methods to define the mechanisms by which tau proteoforms disrupt proteostasis in tauopathies. We hypothesize that tau proteoforms are sufficient to destabilize proteostasis and to result in the accumulation of tau in vulnerable brain regions. To test this hypothesis, we will determine the extent to which MAPT mutations cause impaired tau phenotypes and proteostasis characteristic of tauopathy. We will also generate a systematic genetic interaction map to elucidate connections between MAPT mutations, proteostasis, and associated therapeutic targets. Together, this study will reveal novel mechanisms underlying tauopathy that are driven by specific tau proteoforms and whether therapeutics designed to block specific tau proteoforms impact pathologic events.
Representative Papers:
Acetylated tau inhibits chaperone-mediated autophagy and promotes tau pathology propagation in mice
A farnesyltransferase inhibitor activates lysosomes and reduces tau pathology in mice with tauopathy
Tau Kinetics in Neurons and the Human Central Nervous System
The complex molecular events that underlie the development of Alzheimer’s disease (AD) are poorly understood and are the key to developing targeted therapies. Our group and others have shown that rare variants in the triggering receptor expressed on myeloid cells 2 gene (TREM2) are associated with increased susceptibility to AD. TREM2 encodes a membrane protein that is part of a receptor-signaling complex that modulates inflammatory responses, phagocytosis and cell survival in myeloid cells, such as microglia. However, the specific role of TREM2 in AD pathogenesis remains unclear. CSF sTREM2 levels are increased in patients with symptomatic AD compared to cognitively normal controls. We have recently discovered that common variants in the MS4A locus are a major regulator of CSF sTREM2 levels. Importantly, the same allele associated with higher CSF sTREM2 levels is associated lower AD risk and delayed age at onset. We also identified a second, independent signal in the MS4A locus that encodes MS4A4A p.M159V, which has the opposite effect on CSF sTREM2 levels and AD risk. Our findings that two independent signals in the MS4A gene region have opposing effects on CSF sTREM2 levels and AD risk points to the connection between MS4A and TREM2 biology in AD pathogenesis. The goal of this project is to elucidate the mechanisms by which MS4A genes alter TREM2 function and drive AD pathogenesis. We hypothesize that MS4A4A is involved in TREM2 trafficking and cleavage and that disrupted interaction between MS4A4A and TREM2 leads to microglial dysfunction and neurodegeneration. To test this hypothesis, we will use genomic and biochemical approaches in human brains and stem cell models. The results of this project will provide the mechanistic framework needed to develop treatments that restore or enhance TREM2 functions in order to prevent neurodegenerative disease.
Representative Papers:
The MS4A gene cluster is a key modulator of soluble TREM2 and Alzheimer’s disease risk
Alzheimer’s disease (AD) is a complex and heterogenous condition in which multiple molecular pathways are disrupted in different cell-types and lead to disease. Genetic findings indicate that amyloid-beta protein clearance and degradation pathways, cholesterol metabolism and the immune system are associated with AD etiology. However, the specific mechanism, genes and molecular networks have not yet been completely identified. Single-nuclei transcriptomic (snRNA-seq) data from human brains provides a detailed molecular atlas to study the pathways dysregulated in AD. We propose to deepen our understanding of the genes, network and molecular pathways associated with AD by sequencing a high-number of neuronal and glial cells (approximately 3.3 million cells) from human brain carriers of key genetic mutations and high risk variants, non-carrier sporadic AD cases and neuropath-free controls. We will leverage a unique collection of human tissue from the Dominantly Inherited Alzheimer Network and Knight-ADRC brain banks, and select +220 brains to perform systematic cell- type specific transcriptomic analyses. This is a unique and innovative study designed to analyze cell-specific transcriptomic dysregulation in carriers of high effect risk variants (TREM2 and APOE) and fully penetrant pathogenic mutations in APP/PSEN1/PSEN2 and by comparing them to sporadic AD cases and neuropath-free controls. This is a powerful approach to address disease heterogeneity, and will provide highly informative insights into the biology and pathology of neurodegeneration. Replication of these findings will be performed in snRNA-seq data from induced pluripotent stem cell derived neurons, astrocytes, and microglia-like cells that will be genome edited to add/remove genetic variants, as well as datasets that are being publicly released. Finally, we will create a knowledge portal in which all of the processed snRNA-seq data from our study will be harmonized with that of other research groups to provide a comprehensive molecular atlas that will provide additional insights into the biology and pathology of AD for the entire research community.
Cerebrovascular pathology is present throughout stages of Alzheimer’s Disease and is correlated with cognitive changes. There is strong evidence that vascular dysfunction is a significant driver of neuropathology. Our long- term objective is to understand the function of Alzheimer’s Disease-associated risk genes in vascular cells, their contribution to the development of cerebrovascular pathology and the opportunities to use this information in therapeutic development. There are over 27 Alzheimer’s Disease-associated risk (AD-risk) loci encompassing numerous genetic variants in non-coding and coding regions and hundreds of linked genes. Our overarching hypothesis is that a subset of AD-risk genes impairs vascular function, causing release of inflammatory factors, blood brain barrier (BBB) impairment, and reduced perfusion, thus contributing to neurodegeneration. To address this, we have assembled a multi-disciplinary team with a proven track record of collaboration, including with ADSP and ADGP members, who bring expertise in vascular pathology in dementia, endothelial cell (EC) signaling and EC functional testing, Alzheimer’s Disease genomics, single cell and nuclear transcriptomics, bioinformatics, CRISPR-based gene editing for large scale screening and AD mouse models for in-depth functional assessment in vivo. Notably, we will address differences in gene effects related to the important biological variables, sex and metabolic disease. Men and women differ in their genetic risk for Alzheimer’s Disease, with sex-specific polygenic risk scores providing better prediction of onset, progression, and pathology than pooled-sex scores. Over 80% of individuals with Alzheimer’s Disease have co-morbid metabolic disease, which exacerbates vascular pathology. We have identified the top 50 AD-risk SNPs and 600 AD-associated genes, and these will be targeted for induced pluripotent stem cell (iPSC)-derived endothelial cell (EC) screens by prime editing and CRISPR-based gene inhibition and activation approaches respectively. iPSC-based production of human ECs and mural cells in 2D and 3D models has been optimized and scaled to enable efficient functional testing of the impact of gene changes, including on neuro-vascular interactions in cerebral organoids. Discoveries made in these human cell systems will be validated by an in-depth investigation of gene expression changes in individual ECs and mural cells across a large collection of Alzheimer’s Disease brain samples using single nuclear sequencing. The EC translatome will also be obtained from mouse Alzheimer’s Disease models that incorporate sex and metabolic disease. These diverse datasets will be harmonized and integrated in order to map vascular phenotypes of AD-risk genes and identify critical molecular pathways that are targetable drivers of AD cerebrovascular pathology. These data will add to the breadth of knowledge being gathered by other groups to further elucidate underlying neuronal, glial, microglial, endothelial and mural cell-cell interactions that contribute in a substantial way to the complex architecture of Alzheimer Disease pathology.
Representative Papers:
Meningeal lymphatics affect microglia responses and anti-Aβ immunotherapy
Alzheimer’s disease (AD) is characterized by the accumulation of amyloid-β (Aβ) and neurofibrillary tangles composed of the tau protein in the brain. More than 200 mutations have been identified in amyloid-β precursor protein (APP), presenilin 1 (PSEN1) and presenilin 2 (PSEN2) that cause autosomal dominant forms of AD (ADAD). PSEN1 and PSEN2 form the catalytic domain of the γ-secretase enzyme, which cleaves APP to generate many Aβ proteoforms which can be modified into variants including posttranslational modifications, truncations and sequence variations. Changes in the relative ratios of Aβ42/40 isoforms have been used to predict pathogenicity of ADAD variants. However, we know less about the contribution of other Aβ proteoforms to AD pathogenesis and the utility of the Aβ proteoform signature as a biomarker of mutation status and/or disease course. For example, what are the Aβ pathogenic cause(s) of ADAD? Several Aβ proteoforms support a causal role for AD, including Aβ42, Aβ43, Aβ37, Aβ39 and modifications including pyroglutamate, oxidation, isomerization, and N- and C-terminal truncation. The objective of this study is to define the effects of ADAD mutations and amyloidosis on Aβ proteoform and disease pathogenesis. To meet this objective, we will define mutation and gene-specific effects on Aβ proteoform signatures using novel mass spectrometry approaches in human plasma, CSF, stem cell derived neurons, and brain tissue. We will then determine how Aβ proteoform signatures relate to histologic amyloid plaque structure in human brains. We hypothesize that ADAD mutations produce a common pathogenic Aβ proteoform signature. The rationale for this proposal is that defining the effects of ADAD mutations and amyloidosis on Aβ proteoforms will be critical to define the common pathogenic Aβ signatures which cause AD. This target validation will guide clinical studies, therapeutic strategies and classify future novel ADAD mutations. This work will be performed in collaboration with the Genetics, Biomarker, Clinical, Neuropathology, Imaging, and Biostatistics Cores.

Representative Papers:
Systematic validation of variants of unknown significance in APP, PSEN1 and PSEN2
Discovery and validation of autosomal dominant Alzheimer’s disease mutations
Neurodegenerative diseases result from multifactorial processes that cause pleiotropic changes in the molecular networks that link a host of biological processes, leading to protein aggregation in the brain, and ultimately to the relentless decline in cognition that characterizes most age-related dementing illnesses. Neurodegenerative diseases, such as Alzheimer disease (AD), idiopathic Parkinson’s disease (PD), and frontotemporal lobar degeneration (FTLD) occur by mechanisms in which common or rare variants associated with disease risk are directly inherited or arise sporadically. Human somatic and stem cell models have emerged as a powerful system for modeling the complexities of pathological gene expression, particularly in the early phase of disease, in the context of a non-neoplastic human genome. Further, human stem cells can be differentiated into individual cell types affected in disease, such as neurons, astrocytes, microglia, and oligodendrocytes, as well as 3D “mini-brain” organoids. To this end, we have established a biorepository of stem cell models of AD and related dementias. The collection includes more than 200 human fibroblasts from the Knight ADRC and the Dominantly Inherited Alzheimer Network (DIAN) and induced pluripotent stem cell (iPSC) lines from more than 30 individuals carrying mutations in APP, PSEN1, PSEN2, GRN, MAPT, and risk variants in MAPT, APOE, TREM2, RAB10 and PLD3. Our long-term goal is to develop a set of tools and biomarkers for AD and related dementias. To do this, we will continue to build a biorepository of human somatic and stem cell models. These cells will facilitate the study of basic disease mechanisms, allow for discovery of novel biomarkers, and facilitate drug discovery platforms. We will focus on cell collection that builds on three major areas of strength in the Knight ADRC: (1) contributions of diverse ethnic backgrounds to molecular and cellular biomarkers of AD; (2) genetic and molecular modifiers of age at onset in large families with a dense family history of late onset AD; and (3) comparison of the molecular and cellular biomarkers that are common and unique between autososomal dominant AD and sporadic, late onset AD. Finally, we will make available the human somatic and stem cell lines to the broader research community to revolutionize our understanding of AD and related dementias.
Representative Papers:
A Comprehensive Resource for Induced Pluripotent Stem Cells from Patients with Primary Tauopathies
Human fibroblast and stem cell resource from the Dominantly Inherited Alzheimer Network








